ISO/TS 22583:2019
(Main)Guidance for supervisors and operators of point-of-care testing (POCT) devices
Guidance for supervisors and operators of point-of-care testing (POCT) devices
This document gives guidance for supervisors and operators of point-of-care testing (POCT) services where POCT is performed without medical laboratory training, supervision or support. It includes the key components that should be considered to provide safe and reliable POCT results. Self-testing is excluded from this document.
Titre manque
General Information
Standards Content (Sample)
TECHNICAL ISO/TS
SPECIFICATION 22583
First edition
2019-11
Guidance for supervisors and
operators of point-of-care testing
(POCT) devices
Reference number
ISO/TS 22583:2019(E)
©
ISO 2019
---------------------- Page: 1 ----------------------
ISO/TS 22583:2019(E)
COPYRIGHT PROTECTED DOCUMENT
© ISO 2019
All rights reserved. Unless otherwise specified, or required in the context of its implementation, no part of this publication may
be reproduced or utilized otherwise in any form or by any means, electronic or mechanical, including photocopying, or posting
on the internet or an intranet, without prior written permission. Permission can be requested from either ISO at the address
below or ISO’s member body in the country of the requester.
ISO copyright office
CP 401 • Ch. de Blandonnet 8
CH-1214 Vernier, Geneva
Phone: +41 22 749 01 11
Fax: +41 22 749 09 47
Email: copyright@iso.org
Website: www.iso.org
Published in Switzerland
ii © ISO 2019 – All rights reserved
---------------------- Page: 2 ----------------------
ISO/TS 22583:2019(E)
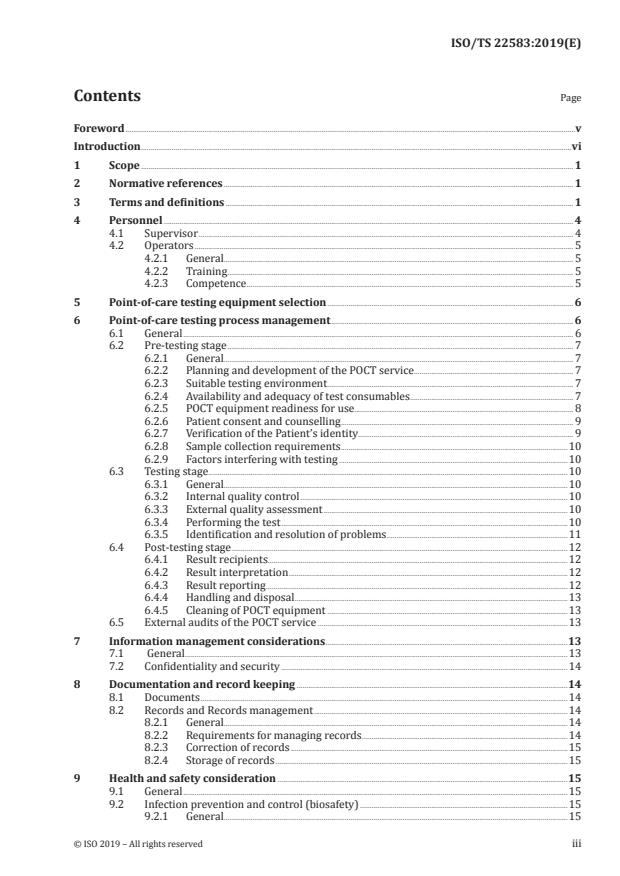
Contents Page
Foreword .v
Introduction .vi
1 Scope . 1
2 Normative references . 1
3 Terms and definitions . 1
4 Personnel . 4
4.1 Supervisor . 4
4.2 Operators . 5
4.2.1 General. 5
4.2.2 Training . 5
4.2.3 Competence . 5
5 Point-of-care testing equipment selection . 6
6 Point-of-care testing process management . 6
6.1 General . 6
6.2 Pre-testing stage . 7
6.2.1 General. 7
6.2.2 Planning and development of the POCT service . . 7
6.2.3 Suitable testing environment . 7
6.2.4 Availability and adequacy of test consumables . 7
6.2.5 POCT equipment readiness for use. 8
6.2.6 Patient consent and counselling . 9
6.2.7 Verification of the Patient’s identity. 9
6.2.8 Sample collection requirements .10
6.2.9 Factors interfering with testing .10
6.3 Testing stage .10
6.3.1 General.10
6.3.2 Internal quality control .10
6.3.3 External quality assessment .10
6.3.4 Performing the test .10
6.3.5 Identification and resolution of problems .11
6.4 Post-testing stage .12
6.4.1 Result recipients.12
6.4.2 Result interpretation .12
6.4.3 Result reporting .12
6.4.4 Handling and disposal .13
6.4.5 Cleaning of POCT equipment .13
6.5 External audits of the POCT service .13
7 Information management considerations .13
7.1 General .13
7.2 Confidentiality and security .14
8 Documentation and record keeping .14
8.1 Documents .14
8.2 Records and Records management .14
8.2.1 General.14
8.2.2 Requirements for managing records .14
8.2.3 Correction of records .15
8.2.4 Storage of records .15
9 Health and safety consideration .15
9.1 General .15
9.2 Infection prevention and control (biosafety) .15
9.2.1 General.15
© ISO 2019 – All rights reserved iii
---------------------- Page: 3 ----------------------
ISO/TS 22583:2019(E)
9.2.2 Use of sharps .16
9.2.3 Personal protection .16
9.2.4 Disposal of waste .16
9.2.5 Hazard analysis .16
9.3 Other health and safety considerations .16
Annex A (normative) Training and competence of operators .17
Annex B (normative) POCT Equipment and selecting the most appropriate test .20
Annex C (informative) Documents and Records .26
Annex D (normative) Internal Quality Control and External Quality Assessment .28
Annex E (informative) Infection prevention and control (Biosafety) .32
Bibliography .35
iv © ISO 2019 – All rights reserved
---------------------- Page: 4 ----------------------
ISO/TS 22583:2019(E)
Foreword
ISO (the International Organization for Standardization) is a worldwide federation of national standards
bodies (ISO member bodies). The work of preparing International Standards is normally carried out
through ISO technical committees. Each member body interested in a subject for which a technical
committee has been established has the right to be represented on that committee. International
organizations, governmental and non-governmental, in liaison with ISO, also take part in the work.
ISO collaborates closely with the International Electrotechnical Commission (IEC) on all matters of
electrotechnical standardization.
The procedures used to develop this document and those intended for its further maintenance are
described in the ISO/IEC Directives, Part 1. In particular, the different approval criteria needed for the
different types of ISO documents should be noted. This document was drafted in accordance with the
editorial rules of the ISO/IEC Directives, Part 2 (see www .iso .org/ directives).
Attention is drawn to the possibility that some of the elements of this document may be the subject of
patent rights. ISO shall not be held responsible for identifying any or all such patent rights. Details of
any patent rights identified during the development of the document will be in the Introduction and/or
on the ISO list of patent declarations received (see www .iso .org/ patents).
Any trade name used in this document is information given for the convenience of users and does not
constitute an endorsement.
For an explanation of the voluntary nature of standards, the meaning of ISO specific terms and
expressions related to conformity assessment, as well as information about ISO's adherence to the
World Trade Organization (WTO) principles in the Technical Barriers to Trade (TBT) see www .iso .org/
iso/ foreword .html.
This document was prepared by Technical Committee ISO/TC 212, Clinical laboratory testing and in
vitro diagnostic test systems.
Any feedback or questions on this document should be directed to the user’s national standards body. A
complete listing of these bodies can be found at www .iso .org/ members .html.
© ISO 2019 – All rights reserved v
---------------------- Page: 5 ----------------------
ISO/TS 22583:2019(E)
Introduction
Due to the ease of use and rapidness of point-of-care-testing (POCT), POCT equipment is widely used as
a tool for making decisions related to the health, management or care needs of patients. Such decisions
can include admission to hospital, evacuation to more appropriate care environments and directed
patient management. There can also be significant civil and/or legal implications that arise from POCT
such as cessation or termination of employment, family court rulings or revocation of bail or parole.
The availability of simple-to-use point of care equipment has led to continuous development in POCT,
examples include testing for diabetes management, blood clotting factors, infectious disease markers,
haemoglobin, white blood cell counts, pregnancy tests, cardiac markers, illicit drug use and performance
enhancing chemical testing.
Whilst examinations of a patient’s body fluids, excreta and tissues have been performed traditionally in
the controlled and regulated environment of a medical laboratory, globally, POCT is increasingly being
performed outside of a traditional laboratory setting and by operators without medical laboratory
support.
Circumstances where POCT testing can occur include but are not limited to hospitals, medical practices,
pharmacies, paramedics, long-term care facilities, outreach clinics in remote and rural settings, in
emergency and natural disasters and community settings such as law enforcement, workplace health
and safety, sporting facilities, academia, the military and public areas such as shopping centres.
As POCT results can be used to make important decisions about patients, it is vital that the equipment
works properly to yield the correct results and that the operators are trained and competent. This
requires that a quality testing structure is provided by supervisors and made available to the operators.
Testing should be of benefit to the patient being tested, if the testing is not performed within a defined
quality testing structure then incorrect results can have a negative effect on the patient in terms of
health outcomes or punitive action taken.
This document has been written in easy to understand language. Its purpose is to provide supervisors
and operators of POCT services guidance for assessing the appropriateness of proposed POCT, test and
equipment selection, as well as skill requirements for technical performance and result interpretation
that will ensure that the reliability, quality and interpretation of the results produced is of a quality
appropriate to the intended use.
It is recommended that manufacturers and their distributors draw this this document to the attention
of purchasers of POCT equipment and encourage them to follow this document.
NOTE 1 The Annexes provide detailed information and add context that is not included in the main body of
this document. Therefore, to appreciate this document fully the reader is encouraged to ensure the relevant
annexes are read in conjunction with main body of this document.
NOTE 2 It is presupposed that procedures are developed in accordance with statutory and regulatory
requirements.
NOTE 3 In some sections readers of this document are referred to medical laboratory professionals. Medical
laboratory professionals with the required competence to offer advice can be found in laboratories adhering to
international standards including ISO 15189, Medical laboratories — Requirements for Quality and Competence
and ISO 22870, Point-of-care testing (POCT) — Requirements for quality and competence.
vi © ISO 2019 – All rights reserved
---------------------- Page: 6 ----------------------
TECHNICAL SPECIFICATION ISO/TS 22583:2019(E)
Guidance for supervisors and operators of point-of-care
testing (POCT) devices
1 Scope
This document gives guidance for supervisors and operators of point-of-care testing (POCT) services
where POCT is performed without medical laboratory training, supervision or support. It includes the
key components that should be considered to provide safe and reliable POCT results.
Self-testing is excluded from this document.
2 Normative references
There are no normative references in this document.
3 Terms and definitions
For the purposes of this document, the following terms and definitions apply.
ISO and IEC maintain terminological databases for use in standardization at the following addresses:
— ISO Online browsing platform: available at https:// www .iso .org/ obp
— IEC Electropedia: available at http:// www .electropedia .org/
3.1
analyte
item that is being measured, tested or calculated
EXAMPLE Glucose, troponin, concaine, HIV antibodies.
3.2
biological reference interval
reference range
normal range
normal value
specified interval of the distribution of values taken from a biological reference population
Note 1 to entry: A reference interval is composed of the values or range for an analyte (3.1) that are expected for
a “healthy person”. They are sometimes called "normal" values. Whilst “normal” ranges can give an indication
about the wellbeing of a patient (3.10), things which should be considered are that a result within the “normal”
range does not necessarily mean the patient (3.10) is healthy, or a result outside of the “normal” range does not
necessarily mean the patient (3.10) is unhealthy. It is also important to note that “normal ranges” can differ from
equipment (3.6) to equipment (3.6) and population to population.
Note 2 to entry: In some cases, such as drugs of abuse testing the normal value should be negative or not detected.
[SOURCE: ISO 15189:2012, 3.4, modified — NOTE 1 to NOTE 4 have been deleted and Note 1 to entry
has been added.]
© ISO 2019 – All rights reserved 1
---------------------- Page: 7 ----------------------
ISO/TS 22583:2019(E)
3.3
clinical handover
patient handover
handover
transfer of professional responsibility and accountability for some or all aspects of care for a patient
(3.10) to another person or professional group on a temporary or permanent basis
Note 1 to entry: Transferring all or part of a patient’s (3.10) care between healthcare providers or locations is a
high-risk situation and a failure in clinical handover is a major source in preventable patient (3.10) harm.
Note 2 to entry: Effective clinical handover, which is structured and standardised, can reduce communication
errors and improve patient (3.10) safety.
Note 3 to entry: A simple example of clinical handover is ensuring critical result notification to an appropriate
person is performed in a timely manner to minimise harm to the patient (3.10).
3.4
competence
demonstrated ability to apply knowledge and skills to produce an accurate POCT result
[SOURCE: ISO 15189:2012, 3.5, modified — “to produce an accurate POCT result” has been added and
“NOTE” has been deleted.]
3.5
critical results
results outside defined limits which may indicate a life-threatening situation and require immediate
notification of the referring doctor
3.6
equipment
any device or apparatus which can be used to perform a POCT (3.11)
Note 1 to entry: Examples include simple colour changing urine test strips for glucose to more complex electronic
hand held or bench top analysers such as glucometers, lipid analysers and alcoholmeters.
Note 2 to entry: For the purposes of this document equipment includes any reagents or consumables required to
perform the test.
3.7
external quality assessment (EQA)
proficiency testing (PT)
process where samples (3.13) of known values are tested periodically and the results are not known to
the operator at the time of testing
Note 1 to entry: The results obtained are then compared against others testing the same sample (3.13) with
the same POCT (3.11) equipment (3.6) type giving the participant the ability to evaluate their performance
against others.
Note 2 to entry: Commercially available EQA programmes are recommended but are not always available. Where
these are not available manufacturers and/or laboratories may be able to offer assistance with sample (3.13)
exchange programs.
3.8
interference factors
a substance or process which falsely alters a test result
Note 1 to entry: Interference can be significant.
Note 2 to entry: Interfering substances can be endogenous (substances found naturally in the patient (3.10)
sample (3.13) such as lipids, proteins, antibodies) or exogenous (substances not naturally found in the patient’s
sample such as drugs, poisons or medications).
2 © ISO 2019 – All rights reserved
---------------------- Page: 8 ----------------------
ISO/TS 22583:2019(E)
Note 3 to entry: The most common interfering factors are haemolysis (the rupturing of red blood cells and the
release of their contents into surrounding fluid (e.g. blood plasma/serum), hyperbilirubinemia (a yellow or green
pigmentation of the blood plasma/serum due to high bilirubin) and lipaemia (an abnormally high concentration
of lipids in the blood, characteristically the blood plasma can appear white or milky in colour due to the presence
of fat).
Note 4 to entry: The type of collection tube can also cause test interference as these often contain additive
components.
3.9
internal quality control (IQC)
quality control (QC)
internal procedure which monitors the testing process to decide if the system is working correctly and
gives confidence that the results are reliable enough to be released
Note 1 to entry: IQC samples (3.13) have known quantities of the analyte (3.1) being tested. The result obtained is
expected to be close to the known value and within an acceptable range. Where results fall outside the acceptable
range action to rectify the issue needs to occur before patients (3.10) are tested.
3.10
patient
individual undergoing POCT (3.11)
Note 1 to entry: For this document the term patient has been used for consistency.
Note 2 to entry: It should be noted that an individual who undergoes POCT (3.11) may not have an ongoing
disease and therefore may not be a patient as such. They can be clients or employees being tested for reasons
other than to receive medical care, such as community screening, pre-employment testing or assessing the use of
performance-enhancing drugs or chemicals.
3.11
point-of-care testing
POCT
near-patient testing
testing that is performed near or at the site of a patient (3.10)
3.12
point of care testing service provider
POCT service provider
individual or organisation responsible for providing POCT (3.11)
3.13
sample
primary sample
specimen
discrete portion of a body fluid (e.g. blood, urine, saliva), breath, hair or tissue taken from the human
body for POCT (3.11) which is assumed to represent the whole patient
Note 1 to entry: In some countries, the terms “specimen” or “primary sample’ are used instead of sample. For
the purpose of this document the terms “sample”, “primary sample” and “specimen” should be considered
interchangeable
Note 2 to entry: The source of blood samples (whether arterial, venous or capillary) is another important
consideration as POCT results for capillary specimens may differ from arterial, venous values for certain tests
and in certain circumstances.
3.14
urgent results
results needed for the care management of a patient within a minimal time period
© ISO 2019 – All rights reserved 3
---------------------- Page: 9 ----------------------
ISO/TS 22583:2019(E)
3.15
validation
process of establishing the performance characteristics and limitations of POCT (3.11) equipment (3.6)
and the identification of the influences which can change these characteristics and to what extent
Note 1 to entry: Which analytes (3.1) it can measure and in which sample (3.13) type (blood arterial, venous or
capillary), plasma, urine) in the presence of which interferences (3.8) are important considerations.
Note 2 to entry: The process for confirming that a method is fit for purpose (is appropriate for its intended use).
3.16
verification
process of demonstrating the performance criteria to which the method has been validated have been
met by the POCT Service provider (3.12) prior to introducing into routine use
4 Personnel
4.1 Supervisor
There shall be an appointed person(s) (supervisor) who has the authority and takes responsibility for,
the quality of the service and is competent to supervise the testing provided.
The supervisor is responsible for the quality, timeliness, accuracy and safe delivery of the POCT which
includes hazard analysis (See 9.2.5).
The supervisor shall define the roles and responsibilities of POCT operators.
The supervisor shall ensure implementation of the following:
— selection of appropriate tests in consultation with a medical professional, when indicated;
— maintaining privacy, safety and confidentiality of personal information and test results of patients
undergoing testing;
— availability of appropriate result interpretation;
— access to advisory services;
— confirmatory testing and/or referral for appropriate or necessary additional testing;
— selection of suitable testing equipment;
— identification and adherence to applicable guidelines;
— performance and review of quality control with corrective actions;
— establishment and maintenance of internal instructions or processes;
— operator training and competency assessment;
— appropriate environment for testing;
— inventory control management processes;
— appropriate and effective clinical handover; and
— appropriate biosafety and infection control procedures.
The supervisor shall ensure procedures are in place and appropriate for the POCT service provided and
that operators adhere to all instructions and procedures relating to POCT.
4 © ISO 2019 – All rights reserved
---------------------- Page: 10 ----------------------
ISO/TS 22583:2019(E)
The supervisor should ensure there is access to medical experts and medical laboratory professionals
to provide consultation as needed.
4.2 Operators
4.2.1 General
There shall be an appointed person(s) (operator) who has been trained and has demonstrated the
competence required to perform testing. A supervisor may also be an operator.
4.2.2 Training
An operator training program shall be implemented that
— describes the key aspects of the testing process including:
— the intent of the testing process;
— its essential steps; and
— the significance of each step;
— ensures the operators can produce reliable results;
— describes the requirements for use of internal quality control and external quality assessment
programs and ensure they are used (if available); and
— states the importance of following policies, procedures and instructions for use.
All operators are required to have successfully completed the training program.
The training program shall be updated when changes to the testing service occur (e.g. new equipment
or procedure is introduced) and operators shall be trained to the new processes.
The training program shall be evaluated periodically for effectiveness.
NOTE Aspects of
...

Questions, Comments and Discussion
Ask us and Technical Secretary will try to provide an answer. You can facilitate discussion about the standard in here.